Wilson’s disease (WD) is an inherited disorder caused by mutations in the ATP7B gene, resulting in the accumulation of copper in various organs such as the liver, brain, cornea, and more. This condition is treatable, but if left untreated, it can lead to permanent disability or even death. Common clinical presentations of WD include hepatic, neurological, and neuropsychiatric variants.
One of the notable eye-related manifestations of WD includes the presence of the ‘Kayser–Fleischer’ (KF) ring in the cornea and the development of a cataract known as the “sunflower cataract.” The KF ring forms due to abnormal copper buildup in the Descemet membrane of the cornea, while the sunflower cataract is a result of copper deposition beneath the lens capsule. Recent studies have also identified copper deposits and related effects on the retina and optic nerve using advanced techniques like electroretinography and anterior segment optical coherence tomography (OCT). OCT is a high-resolution imaging method that provides cross-sectional images of various eye tissues using long-wavelength light beams, allowing for three-dimensional measurements.
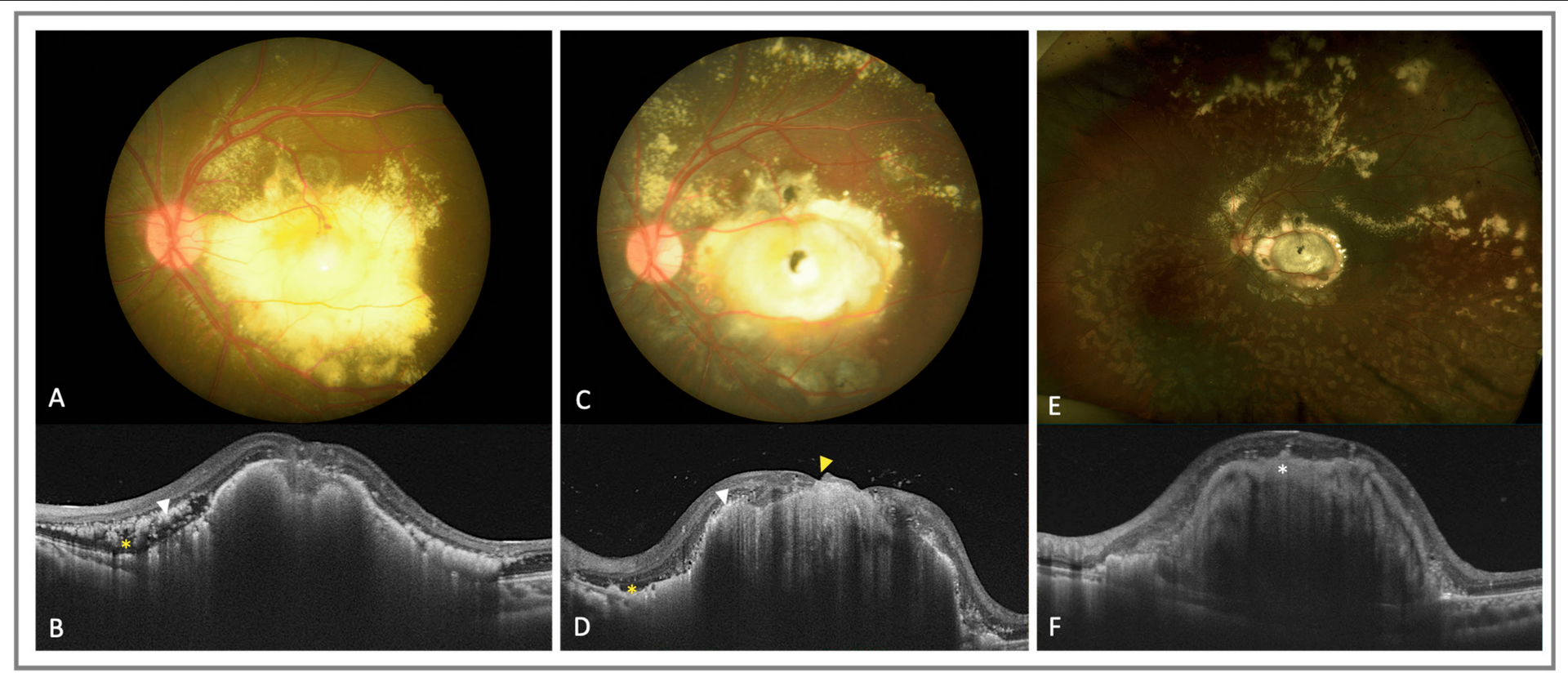
A recent publication in the Annals of Indian Academy of Neurology by Bhattacharya et al. reviewed 16 WD patients who underwent OCT during follow-up visits. The researchers utilized Spectral-domain OCT to measure macular and retinal nerve fiber layer (RNFL) thickness and compared the data with a group of 14 healthy individuals. Measurements were taken at various locations in the macula and in specific quadrants.
The study found significant differences in macular thickness, particularly in the ganglion cell and inner plexiform layer complex (GCIP) and the outer nuclear layer with the photoreceptor layer (ONL + PRL), when comparing patients with WD to healthy controls. Additionally, their analysis revealed a significant relationship between clinical factors (disease duration, GAS-WD score) and OCT measurements (macular thickness and RNFL in superior and inferior quadrants).

The results indicated that WD patients had lower intraocular pressure and reduced RNFL thickness compared to healthy individuals. Furthermore, it was observed that macular thickness decreased before RNFL thickness in the early stages of the disease, suggesting that macular thickness could serve as an early biomarker for WD.
OCT is a valuable non-invasive tool for studying retinal changes in WD patients, aiding in the assessment of neurodegeneration, therapy monitoring, and prognosis. The thinning of the ganglion cell layer (GCL) and outer plexiform layer (OPL) may be indicative of disease progression or therapeutic effectiveness in WD.